Platelet-Rich Plasma Stays Quietly Popular Despite Neglect
Fact: PRP Treatments Are Highly In-Demand
According to research, PRP treatments are one of the most in-demand treatments available in healthcare. This is impressive considering the following challenges PRP faces:
- Lack of Support from the Medical Industry: PRP is not backed by big pharma, meaning no extensive research or marketing is funded.
- Absence of Lobbying by Medical Associations: There are no medical associations working to increase awareness of PRP.
- No Insurance Reimbursements: Insurance companies do not reimburse PRP treatments, making it difficult to get patients to pay for a treatment that is relatively “unproven.”
- Rising Costs: In 2006, a PRP treatment cost $450. Today, it costs $800, with the cheapest being $650.
Despite these obstacles, the demand for PRP treatments remains robust.
The Future of PRP
We believe the best of PRP is yet to come. A breakthrough study could propel PRP into mainstream hospitals and clinics. The most significant growth in PRP is currently happening in Asia, rooted in fundamental healing theory.
The Healing Power of PRP
The growth of PRP can be attributed to its fundamental healing properties:
- Increased Platelets: More platelets mean more growth factors and cytokines, leading to enhanced healing.
- Natural Healing Mechanism: Our body’s natural healing mechanism operates with 150,000/ul-350,000/ul platelets in blood. Using PRP amplifies this number by 3X to 5X, translating to better healing.

Platelet-Rich Plasma Trends
PRP can be used to promote the healing of injured tendons, ligaments, muscles, and joints, and is applied to various musculoskeletal problems. Regular studies test its effectiveness. One landmark study involved double-blind randomized controlled trials to see the effect of PRP on patients with chronic low back pain caused by torn discs. The study found that 60% of the patients felt significant improvements, with some even being cured.
Platelet-Rich Plasma Variants
There are several types of PRP variants:
- Plasma Rich in Growth Factors (PRGF)
- Plasma Rich in Platelets and Growth Factors (PRPGF)
- Platelet-Rich Plasma (PRP)
- Platelet Poor Plasma (PPP)
- Plasma Rich in Platelets and Rich in Leukocytes (LR-PRP)
- Plasma Rich in Platelets and Poor in Leukocytes (LP-PRP)
- Platelet-Rich Fibrin Matrix (PRFM)
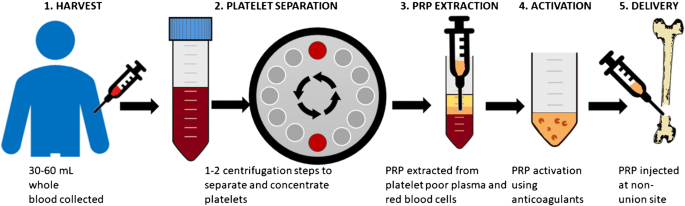
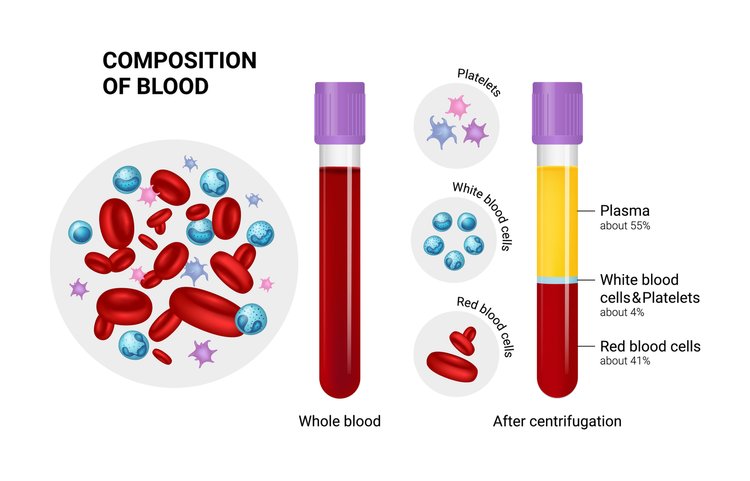
All of them involve plasmapheresis—the two-stage centrifugation process to separate platelets from blood. The industry has yet to standardize which variant to use, but we believe the confusion will clear up in 3-5 years.
Bio-Factors at Play in PRP
Regardless of the PRP variant used, the following bio-factors are at play:
- Growth Factors: TGF-B, PDGF, IGF-I,II, FGF, EGF, VEGF, ECGF
- Adhesive Proteins: Fibrinogen, Fibronectin, Vitronectin, Thrombospondin-1
- Clotting & Anti-Clotting Factors: Proteins, Antithrombin, Plasminogen, Proteases, Antiproteases
How Platelet-Rich Plasma Actually Works
PRP is commonly used for wound healing and pain management because platelets aid coagulation, act as a biological glue, and support stem or primary cell migration. They also help restore hyaluronic acid, accelerate collagen synthesis, and increase cartilage matrix.
Platelets delivered in a clot can immediately act as a scaffold to enable the healing process. 95% of bio-active proteins are released within 1 hour of injecting PRP, and platelets continue to release growth factors for 7-10 days. Thus, it’s recommended to re-inject PRP every 7 days.
Why Patients Choose PRP Despite the Cost
Patients are willing to pay out of pocket for PRP treatments despite insurance companies not covering it because:
- Effectiveness: The treatment works.
- Natural and Side-Effect-Free: There is nothing else as natural and side-effect-free as PRP.
PRP for Osteoarthritis
Consider osteoarthritis, which affects 27 million Americans. When doctors started doing PRP treatments for their osteoarthritis patients, a large majority experienced no further cartilage loss. This suggests PRP should be the default first-line treatment for osteoarthritis across the country.
PRP for Hair Loss and Cosmetic Applications
PRP also has significant potential in treating hair loss and cosmetic facial applications. Studies have shown reduced hair loss and increased hair density, with patients expressing high satisfaction levels.
The Growing PRP Market
The PRP market is expected to hit $126 million in 2016, a 180% increase over the 2009 figure of $45 million. For osteoarthritis alone, if all 27 million Americans received 1 PRP shot a year at a conservative $400 per treatment, it would be a $10 billion market.
PRP for Tennis Elbow
PRP is also known to work well for Tennis Elbow, which affects 1% to 3% of the overall population and up to 50% of tennis players.
Insurance Coverage for PRP
Getting PRP covered by insurance could significantly expand the market and help heal millions of patients more naturally and effectively. It could also save insurance companies money by reducing the need for more expensive interventions like surgery.
Challenges and the Future of PRP
The vast scope of PRP treatment calls for urgent structure and guidelines. There are some 20+ conditions where researchers have found it helpful. Proving its efficiency in all these areas is a daunting task, but we will get there with enough funding and standardized procedures.
Conclusion
Despite being classified as “unproven,” PRP has vast potential. With the right number of platelets, platelet activation, and cytokine release, PRP can consistently deliver positive outcomes. Although there is still uncertainty over the number of injections, timing, and delivery method, widespread adoption will eventually lead to a more structured approach.
Let’s hope the first glimpses of this structure will arrive soon. In 2015, the world saw approximately 1 million knee arthroplasties for osteoarthritis, costing $25 billion. How many of these patients could have benefited from PRP early on?
- Published in Corporate News / Blog
Platelet-Rich Plasma For Melasma — Will It Fade Forever?
For most women, a tiny pimple on the face is enough to ruin their day. Or week. Even the slightest imperfection that may have a 1% chance of getting noticed by others will freak them out. For these women, Melasma is their darkest nightmare. It’s a pretty common issue, a result of exposure to the sun, that causes brown patches on the face. Permanent patches, I should add.
If you’re suffering from Melasma, the road to “recovery” usually looks like this:
- You hope that it’ll fade away.
- Your friend suggests you try apple cider vinegar and lemon juice treatment.
- Slightly disappointed.
- You visit a dermatologist who’ll prescribe a bleaching cream (hydroquinone or similar).
- Full-on disappointment.
- You Google the hell out of the topic.
- Overwhelm.
- Concealers and makeup become your best friend.
At this point, no one can convince you there is a treatment for getting rid of melasma. Trying more and more treatments only runs the risk of making the condition worse. So what would you do?
What About Platelet-Rich Plasma For Melasma?
According to recent Turkish and Malaysian studies, Platelet-Rich Plasma is showing great promise for melasma. The one good thing about PRP for Melasma is the fact that PRP won’t make the condition worse unlike IPL, Fraxel, or other treatments. So that’s one of the treatments you can confidently try without worry. It’s like getting a natural facial treatment that has a whole lot of potential benefits even if it didn’t help cure melasma.
PRP injections work by supplying growth factors to reduce the pigmentation. And being an independent treatment with no downtime, it can be done in conjunction with conventional treatments for melasma to add and enhance the effects. There are more than 30 bioactive substances in Platelet-Rich Plasma that have separate roles like increasing skin volume and adding new blood vessels to name a few.

Platelet-Rich Plasma with Microneedling
This is the most common combination for Platelet-Rich Plasma therapy. Here’s a video of Dr. Michael Somenek performing a PRP injection on a patient of his immediately after microneedling. The combination is known to have produced results for a lot of varieties of skin pigmentation issues that it’d not be wise for anyone to ignore it for melasma, especially when creams and peels didn’t help. More important is PRP’s ability to stimulate collagen production in the area so it tightens the pores and makes your skin glowing.
Why Platelet-Rich Plasma?
PRP is primarily a healing vehicle. It needs to be injected into the membrane below the skin. The way it works is by supplying the underlying skin membrane with collagen and tenascin stimulated by the transforming growth factors in PRP. These growth factors also promote the formation of new blood vessels that in some cases results in the disappearance of spider veins.
The released growth factors (mainly platelet-derived growth factor (PDGF), epidermal growth factor (EGF), vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), and transforming growth factor-beta (TGF-ß)) can stimulate the proliferation of fibroblasts and epidermal cells, and collagen synthesis. In addition, the transforming growth factor-beta (TGF-ß) has been proven to inhibit melanogenesis — or reverse skin pigmentation — the exact opposite effect of exposure to UV-B radiation.
Typically, patients see excellent results with 2-3 PRP injections in the first 3 months. And clinical studies have shown that it will maintain after 6 months. However, Melasma is known to recur even after successful treatments. So you must take precautions against it by using sunscreen with broad-spectrum protection and an SPF of 30 or higher. And avoid skincare products that are harsh as they can exacerbate melasma.
- Published in Corporate News / Blog
Platelet-Rich Plasma For Melasma — Will It Fade Forever?
For most women, a tiny pimple on the face is enough to ruin their day. Or week. Even the slightest imperfection that may have a 1% chance of getting noticed by others will freak them out. For these women, Melasma is their darkest nightmare. It’s a pretty common issue, a result of exposure to the sun, that causes brown patches on the face. Permanent patches, I should add.
If you’re suffering from Melasma, the road to “recovery” usually looks like this:
- You hope that it’ll fade away.
- Your friend suggests you try apple cider vinegar and lemon juice treatment.
- Slightly disappointed.
- You visit a dermatologist who’ll prescribe a bleaching cream (hydroquinone or similar).
- Full-on disappointment.
- You Google the hell out of the topic.
- Overwhelm.
- Concealers and makeup become your best friend.
At this point, no one can convince you there is a treatment for getting rid of melasma. Trying more and more treatments only runs the risk of making the condition worse. So what would you do?
What About Platelet-Rich Plasma For Melasma?
According to recent Turkish and Malaysian studies, Platelet-Rich Plasma is showing great promise for melasma. The one good thing about PRP for Melasma is the fact that PRP won’t make the condition worse unlike IPL, Fraxel, or other treatments. So that’s one of the treatments you can confidently try without worry. It’s like getting a natural facial treatment that has a whole lot of potential benefits even if it didn’t help cure melasma.
PRP injections work by supplying growth factors to reduce the pigmentation. And being an independent treatment with no downtime, it can be done in conjunction with conventional treatments for melasma to add and enhance the effects. There are more than 30 bioactive substances in Platelet-Rich Plasma that have separate roles like increasing skin volume and adding new blood vessels to name a few.
Platelet-Rich Plasma with Microneedling
This is the most common combination for Platelet-Rich Plasma therapy. Here’s a video of Dr. Michael Somenek performing a PRP injection on a patient of his immediately after microneedling. The combination is known to have produced results for a lot of varieties of skin pigmentation issues that it’d not be wise for anyone to ignore it for melasma, especially when creams and peels didn’t help. More important is PRP’s ability to stimulate collagen production in the area so it tightens the pores and makes your skin glowing.
Why Platelet-Rich Plasma?
PRP is primarily a healing vehicle. It needs to be injected into the membrane below the skin. The way it works is by supplying the underlying skin membrane with collagen and tenascin stimulated by the transforming growth factors in PRP. These growth factors also promote the formation of new blood vessels that in some cases results in the disappearance of spider veins.
The released growth factors (mainly platelet-derived growth factor (PDGF), epidermal growth factor (EGF), vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), and transforming growth factor-beta (TGF-ß)) can stimulate the proliferation of fibroblasts and epidermal cells, and collagen synthesis. In addition, the transforming growth factor-beta (TGF-ß) has been proven to inhibit melanogenesis — or reverse skin pigmentation — the exact opposite effect of exposure to UV-B radiation.
Typically, patients see excellent results with 2-3 PRP injections in the first 3 months. And clinical studies have shown that it will maintain after 6 months. However, Melasma is known to recur even after successful treatments. So you must take precautions against it by using sunscreen with broad-spectrum protection and an SPF of 30 or higher. And avoid skincare products that are harsh as they can exacerbate melasma.
- Published in Corporate News / Blog
tem Cell Platelet-Rich Plasma: The Best Regenerative Therapy?
To understand why stem cell platelet-rich plasma or co-transplantation of adipose-derived mesenchymal stem cells (ADSC) and PRP is such a remarkable idea in regenerative medicine, let’s spend a little time looking at the mechanics of PRP.
Platelet-Rich Plasma’s Role as Repairmen
The one thing that makes Platelet-Rich Plasma a hero in several fields (if not all) of medicine is the fact that the diverse growth factors in it are able to stimulate stem cell proliferation and cell differentiation (the factors that determine effective tissue regeneration and healing) on any part of the body. These growth factors are abundant in the blood and act as the natural repairmen of tissues. In the perfect scenario, there’s plenty of blood flow to every part of the body, and these “repairmen” are always on-call to address any healing needs that may arise. However, if the injured area has a poor blood supply — especially areas that constantly move like tendons, ligaments, and joints — demand for these repairmen can outgrow supply. Meaning, healing (or regeneration of tissues) is put on hold till further repairmen are available.
The train of Platelet-Rich Plasma then arrives with enough of these repairmen to warrant the resumption of healing. There’s another part of this picture we haven’t talked about so far: stem cells.
Stem Cells as the Raw Materials for PRP
As far as Platelet-Rich Plasma and its growth factors are concerned, they are mere repairmen. They can’t do the work by themselves. They need the basic raw materials to work with. And that raw material here is stem cells. Stem cells are the ones actually being regenerated to form new tissues for healing.
Supplying Both PRP and Stem Cells for Regeneration
Stem cells are the only raw materials that PRP works with for regeneration. These are like the fundamental building blocks of all other cells. These cells can be guided into becoming specialized cells under the right conditions. In addition, they can also divide themselves to form new stem cells or new specialized cells. So for Platelet-Rich Plasma to work well, it needs to be applied to an area with lots of stem cells like the heart, liver, blood vessels, etc. Incidentally, Platelet-Rich Plasma’s healing properties were first discovered by cardiac surgeons who played with concentrated blood for faster healing of the heart after surgery, and it showed tremendous promise because stem cells are abundant in heart tissues. But what if healing is needed in an area where there are not many stem cells?
With the new developments in stem cell technology, that can be solved too. Because now we can supply the stem cells to areas where there are less like the joints, ligaments, and tendons. For this, scientists usually use “mesenchymal stem cell” or MSCs. These are cells isolated from stroma and can differentiate to form adipocytes, cartilage, bone, tendons, muscle, and skin. The easiest way is to harvest it from adipose tissue or fat that we call Adipose-derived mesenchymal stem cells or ADSC.
The Future of Stem Cell Platelet-Rich Plasma
In regions with hypoxia (poor blood supply) like joints, meniscus tissue, rotator cuff, spinal discs, etc., the supply of platelets (and therefore growth factors) as well as the stem cells are limited. So what if we supplied both the stem cells and Platelet-Rich Plasma for triggering the regeneration process? That’s the question these Japanese scientists answered in their research. Here’s another group of scientists who took on the same challenge.
They used Adipose-derived mesenchymal stem cells (ADSC), which are known for their ease of isolation and extensive differentiation potential. These researchers noted that these stem cells often can’t survive in areas of local hypoxia, oxidative stress, and inflammation – thereby making them ineffective. However, when Platelet-Rich Plasma (or thrombin-activated PRP) is added to ADSC, it kept them alive for prolonged periods and the growth factors in the Platelet-Rich Plasma triggered cell differentiation and proliferation more easily.
Why This Exact Combination Is the Future
Done this way, both Adipose-derived mesenchymal stem cells (ADSC) and Platelet-Rich Plasma are raw materials for healing that’s already available in plenty in almost everyone (there are exceptions of course). That means, for complete healing to take place, this combination treatment, still in its very primitive stage of development, may have the potential to replace expensive synthetic drugs that carry complex unexplained side effects. The procedure takes our body’s natural healing agents — stem cells from body fat and PRP from blood — and then injects them inside the knee or other joints (or other areas where they are insufficient) for regeneration. Isn’t that like the most wonderful thing ever?
Whether it’s a cartilage cell, a bone cell, or a collagen cell for ligaments and tendons that need to be healed, all you need is a same-day procedure by a local, but specialized doctor, using the natural ingredients of the body. I believe this special combo is a huge win for Platelet-Rich Plasma.
The Challenges for Growing Adoption of This Treatment
We know Platelet-Rich Plasma has safe, yet high-speed recovery potential with its multiple growth factors. And it is effective in regenerative healing of cartilage injuries – the toughest injuries to heal – as well as Osteoarthritis. However, the challenges are Platelet Quality. We need to somehow ensure the Platelet-Rich Plasma quality is uniform. Currently, it varies from two to several fold above baseline concentration based on the donor’s physical condition.
Next, we need to identify the exact PRP growth factors that promote ADSC proliferation. Scientists believe growth factors such as basic fibroblast growth factor (bFGF), epidermal growth factor, and platelet-derived growth factor stimulate stem cell proliferation while some growth factors under certain conditions are known to inhibit the process. The percentage of PRP matters too. Scientists have tested 5 percent, 10 percent, 15 percent, and 20 percent Platelet-Rich Plasma in ADSC.
The Only Treatment in Modern Medicine for Cartilage Regeneration
The bottom line is that Stem Cell Platelet-Rich Plasma or ADSC + PRP procedure is the only treatment in modern medicine that has shown cartilage regeneration. So it’s too important to ignore. And it could be one of the greatest advances that science has brought to the millions of people suffering from serious pain in their joints, knee, and spine as well as people suffering from all kinds of tendon diseases and injuries.
To understand why stem cell platelet-rich plasma or co-transplantation of Adipose-derived mesenchymal stem cells and PRP, is such a remarkable idea in regenerative medicine, let’s spend a little time looking at the mechanics of PRP.
- Published in Corporate News / Blog
Global Stem Cells Group and Adimarket to Represent Magellan in Latin America and Middle East
Global Stem Cells Group and its subsidiary Adimarket named representatives for Magellan Autologous Platelet Separator in Latin America and Middle East.
MIAMI, Nov. 29, 2017— Global Stem Cells Group (GSCG), a world leader in stem cell and regenerative medicine, and its subsidiary Adimarket have been named to represent the Magellan Autologous Platelet Separator in Latin America and Middle East.
Developed by Arteriorcyte Medical Systems, a leading medical device company headquartered in Hopkinton, Mass., the Magellan Autologous Platelet Separator is a high-tech, automated dual spin processing system designed for use in clinical laboratories or intraoperatively at the point-of-care for safe and rapid preparation of high-quality, platelet-rich plasma (PRP) as well as platelet poor plasma (PPP).
Global Stem Cells Group CEO Benito Novas says the Magellan system is a perfect fit for GSCG and Adimarket’s ever-growing list of high-tech regenerative medicine products and equipment, made available to physicians and qualified practitioners through the Adimarket online store.
“We share Arteriocyte’s commitment to research and development of blood component technology to advance treatments that benefit patients in the field of regenerative medicine,” Novas says. “The Magellan system furthers GSCG’s drive to invest in platelet separation technologies that focus on the development of new surgical applications for PRP and elevates these technologies to the next level.”
The fully-automated Magellan system is specifically designed to fractionate blood at bedside without a need for manual manipulation. At the end of its cycle, the Magellan PRP is delivered into a collection syringe, ready for immediate application.
As an industry leader, Adimarket added the Magellan Autologous Platelet Separator System to its online regenerative medicine store to allow physicians to meet the specific needs of each patient with fully customizable product volumes and platelet concentrations. The system can be programmed to deliver a volume of 3 – 10 mL from each processing cycle, allowing practitioners to customize the concentration per mL within the PRP. The Magellan system is approved for three processing cycles per disposable separation chamber, allowing for a maximum of 30 mL of product.
For more information, visit the Adimarket regenerative medicine online store website, email info@stemcellsgroup.com, or call 305-560-5337.
About Global Stem Cells Group:

Global Stem Cells Group (GSCG) Global Stem Cells Group (GSCG) is a worldwide network that combines seven major medical corporations, each focused on furthering scientific and technological advancements to lead cutting-edge stem cell development, treatments, and training. The united efforts of GSCG’s affiliate companies provide medical practitioners with a one-stop hub for stem cell solutions that adhere to the highest medical standards.
Global stem cell’s mission is to be the largest recognized stem cell and regenerative medicine network in the world.
About Adimarket:
 Adimarket, Inc., a division of the Global Stem Cells Group, is a one-stop, cost-competitive online marketplace for quality regenerative medicine equipment and supplies for physicians and health care professionals.
Adimarket, Inc., a division of the Global Stem Cells Group, is a one-stop, cost-competitive online marketplace for quality regenerative medicine equipment and supplies for physicians and health care professionals.Adimarket was founded to provide practitioners the tools they need to practice regenerative medicine in a medical office setting. Motivated by a firm belief in the impact stem cell medicine can have when dispensed in a doctor’s office, Adimarket provides physicians with the tools they need to provide patients with cutting-edge treatments.
About Arteriorcyte Medical Systems:
 Arteriocyte Medical Systems, Inc. is a leading medical device company committed to developing and marketing novel medical products to help patients heal faster. Established in 2007 by Arteriocyte, Inc. and DW Healthcare Partners, Arteriocyte Medical Systems is devoted to providing innovative solutions to patients and medical professionals to address serious unmet medical needs particularly in cardiac, orthopedic and vascular surgeries.
Arteriocyte Medical Systems, Inc. is a leading medical device company committed to developing and marketing novel medical products to help patients heal faster. Established in 2007 by Arteriocyte, Inc. and DW Healthcare Partners, Arteriocyte Medical Systems is devoted to providing innovative solutions to patients and medical professionals to address serious unmet medical needs particularly in cardiac, orthopedic and vascular surgeries.###
Magellan Autologous platelet separator
- Published in Press Releases






