Introduction to PRP in Regenerative Medicine
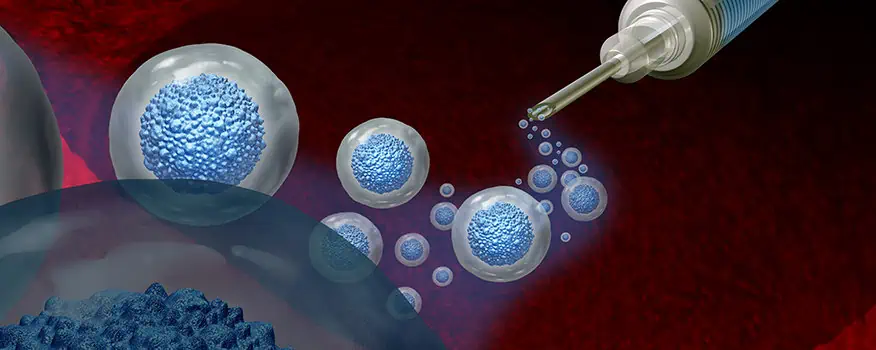
In the regenerative medicine specialty, we have been active for about 8 years. Like many others, we started by using Platelet-Rich Plasma (PRP). We learned about it, were fascinated by it, and treated our patients with it. Patients loved it, and so did we.
PRP, if obtained and used correctly, is a powerful tool to implement in any medical practice, especially when dealing with the elderly, osteoarthritis, wear and tear of tendons and ligaments, and loss of vitality. PRP is also frequently used in plastic and reconstructive surgery for wound care, scar improvement, and overall skin rejuvenation.
How PRP Works
But why does PRP work, and how?
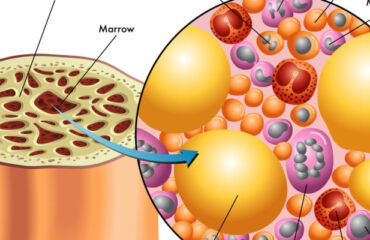
We are all familiar with platelets. They have significant power and influence over tissue regeneration, and by concentrating them in a blood sample, we can obtain signaling proteins, cytokines, and growth factors. If we add white blood cells to the mix, we get what is called L-PRP (leukocyte-rich PRP), making that “soup” even more interesting.
What is Photobiomodulation?
To harness the power of these bioactive substances, we need to coax the cells into releasing them. Normally, platelets are activated by the addition of calcium or by contact with collagen. However, several studies have demonstrated the influence of low-intensity laser on the activity of some cells. This effect is called “photobiomodulation.” This modality uses non-ionizing light sources, like LEDs or Helium-Neon lasers, to produce photochemical events at various biological scales. It has been demonstrated that this light reacts with the enzyme cytochrome c oxidase, which is paramount in mitochondrial processes.
Effects of Photobiomodulation on Cellular Cultures
Several scientists studied this light and its effects on cellular cultures. They found that cells proliferate more when exposed to low-level laser and showed increased viability.
We compared the levels of cytokines and growth factors in an irradiated sample and a non-irradiated one. Some growth factors even tripled in concentration after laser exposure. The famous interleukin-10, an anti-inflammatory protein, doubled in levels, and endorphins were released in high levels.
Benefits of Photobiomodulation
The photobiomodulation process has been established to provide extraordinary benefits in pain management, inflammation reduction, immunomodulation, and promotion of wound healing and tissue regeneration. It plays a fundamental part in our protocols.
Isn’t it all sort of amazing?
We’ll see you in the next blog. Keep your cells healthy!