NK Therapy: The Future of Anti-Aging and Immune System Support
NK cells are a crucial part of the innate immune system. They are responsible for detecting and destroying cells that are infected with viruses or have become cancerous. Their ability to recognize stressed cells in the absence of antibodies and MHC, which marks them for destruction, makes them unique.
What is NK Therapy?
NK therapy involves the infusion or stimulation of NK cells to enhance the body’s natural immune response. This therapy can be autologous (using the patient’s own cells) or allogeneic (using cells from a donor). The goal is to increase the number and activity of NK cells to fight diseases and improve overall health.
Mechanisms of NK Cell Activation
NK cells can be activated by cytokines, such as IL-2 and IL-15, which enhance their proliferation and cytotoxic activity. Understanding these mechanisms is essential for optimizing NK therapy protocols.
NK Therapy and Aging: An Overview
Aging is associated with a decline in immune function, known as immunosenescence. NK therapy aims to counteract this decline by replenishing and activating NK cells, potentially slowing down the aging process and improving health span.
The Role of NK Cells in the Immune System
NK cells are involved in the early defense against infections and tumors. They produce cytokines that regulate the immune response and work synergistically with other immune cells to maintain homeostasis and protect against diseases.
Clinical Applications of NK Therapy
NK therapy has been explored in various clinical settings, including cancer treatment, viral infections, and autoimmune diseases. Its applications are expanding as research uncovers more about the therapeutic potential of NK cells.
Benefits of NK Therapy for Anti-Aging
- Enhanced Immune Function: By boosting NK cell activity, the immune system can more effectively combat infections and malignancies.
- Reduction in Age-Related Diseases: NK therapy may help reduce the incidence of diseases that commonly increase with age, such as cancer and viral infections.
- Improved Skin Health: NK cells can target senescent cells, which accumulate with age and contribute to skin aging.
How NK Therapy Enhances Immune Function
NK therapy enhances immune function by increasing the number and activity of NK cells, which are pivotal in recognizing and destroying infected or cancerous cells. This boost in immune surveillance can lead to better overall health and disease resistance.
Research and Development in NK Therapy
Ongoing research aims to optimize NK cell expansion, activation, and delivery methods. Advances in genetic engineering and biomanufacturing are also being explored to enhance the efficacy and safety of NK therapy.
Comparing NK Therapy with Other Anti-Aging Treatments
While traditional anti-aging treatments focus on cosmetic improvements, NK therapy addresses aging at the cellular level, potentially offering more profound and long-lasting benefits. It complements other treatments by targeting the root causes of aging.
The Future of NK Therapy in Medicine
The future of NK therapy looks promising, with potential applications in a wide range of diseases beyond aging and immune support. Advances in personalized medicine and biotechnology are expected to enhance the effectiveness of this therapy.
Conclusion: The Promise of NK Therapy
NK therapy represents a novel and promising approach to anti-aging and immune system support. By harnessing the power of natural killer cells, this therapy offers a new frontier in medicine, with the potential to improve health outcomes and quality of life.
- Published in Corporate News / Blog
Peptides in Regenerative Medicine: Unlocking Longevity and Wellness
Regenerative medicine is an evolving field that leverages the body’s ability to heal and regenerate itself. Among the various tools in regenerative medicine, peptides have gained significant attention for their potential to promote tissue repair and enhance overall health. This article delves into the role of peptides in regenerative medicine, their benefits, and their applications.
What Are Peptides?
Peptides are short chains of amino acids, which are the building blocks of proteins. They are naturally occurring in the body and play crucial roles in various physiological processes, including hormone production, immune function, and tissue repair. Unlike proteins, peptides are smaller and can penetrate cells more easily, making them highly effective in targeted therapies.
How Peptides Work in Regenerative Medicine
Peptides work by signaling cells to perform specific functions. In regenerative medicine, peptides can promote cell growth, stimulate collagen production, reduce inflammation, and enhance wound healing. These properties make them invaluable in treating various conditions, from skin injuries to degenerative diseases.
Types of Peptides Used in Regenerative Medicine
- Growth Hormone Releasing Peptides (GHRPs): These peptides stimulate the release of growth hormone, which is essential for tissue repair and regeneration.
- Thymosin Beta-4 (TB-500): Known for its wound healing properties, TB-500 can accelerate recovery from injuries and reduce inflammation.
- BPC-157: Derived from a protein in the stomach, BPC-157 promotes healing of muscles, tendons, and ligaments.
- Collagen Peptides: These peptides support skin elasticity and joint health by boosting collagen production.
- GHK-Cu (Copper Peptide): Enhances skin repair, reduces inflammation, and promotes wound healing.
- SS-31: A mitochondrial-targeted peptide that protects cells from oxidative stress and enhances cellular energy.
- MOTS-C: Enhances mitochondrial function, promotes metabolic health, and has anti-aging effects.
- Tesamorelin: Stimulates growth hormone release, improves body composition, and is used in the treatment of lipodystrophy.
- Ipamorelin: Promotes muscle growth and recovery, with fewer side effects compared to other growth hormone secretagogues.
- Melanotan II: Often used for skin tanning, it also has benefits for sexual wellness.
- Semaglutide: A peptide used for weight management and type 2 diabetes, known for its ability to suppress appetite.
- Tirzepatide: A dual-action peptide that regulates blood sugar levels and promotes weight loss.
- Epithalon: Known for its potential anti-aging properties, improving sleep quality, and promoting longevity.
Applications of Peptides in Regenerative Medicine
- Wound Healing: Peptides like TB-500, BPC-157, and GHK-Cu are effective in speeding up the healing process of acute and chronic wounds.
- Anti-Aging: Peptides such as collagen peptides, GHK-Cu, and Epithalon can improve skin elasticity, reduce wrinkles, and promote a youthful appearance.
- Muscle and Joint Repair: Athletes and individuals with musculoskeletal injuries can benefit from peptides like TB-500, BPC-157, and Ipamorelin that promote muscle growth and repair.
- Immune Modulation: Certain peptides can modulate the immune system, reducing inflammation and enhancing immune response.
- Sexual Wellness: Peptides like Melanotan II and PT-141 can enhance sexual function and libido.
- Longevity: Peptides such as Epithalon and MOTS-C are being studied for their potential to extend lifespan and improve overall health.
- Beauty: Collagen peptides, GHK-Cu, and other skin-targeting peptides can improve skin texture, elasticity, and hydration.
- Weight Loss: Peptides like Semaglutide, Tirzepatide, CJC-1295, and Ipamorelin can aid in fat loss and improve body composition.
- Metabolic Health: MOTS-C and Tesamorelin help in enhancing metabolic functions and overall energy levels.
Benefits of Peptide Therapy
- Targeted Action: Peptides can be designed to target specific tissues or cells, reducing the risk of side effects.
- Natural and Safe: Since peptides are naturally occurring in the body, they are generally well-tolerated and safe.
- Versatility: Peptides can be used to treat a wide range of conditions, making them versatile tools in regenerative medicine.
- Non-Invasive: Peptide therapy often involves simple injections or topical applications, offering a non-invasive treatment option.
Clinical Evidence and Research
The efficacy of peptides in regenerative medicine is supported by numerous studies. For instance, research has shown that BPC-157 accelerates tendon healing and reduces inflammation in animal models. Similarly, TB-500 has demonstrated potential in promoting cell migration and wound healing. Studies on GHK-Cu indicate its effectiveness in skin repair and reducing inflammation. Epithalon has shown promise in improving sleep quality and promoting longevity. Semaglutide and Tirzepatide have shown promising results in weight management and diabetes treatment.
Future Directions in Peptide Research
The future of peptides in regenerative medicine is promising, with ongoing research exploring new peptides and their applications. Advances in peptide synthesis and delivery methods are expected to enhance their therapeutic potential further.
Conclusion
Peptides represent a powerful tool in the field of regenerative medicine, offering targeted, natural, and versatile treatment options for various conditions. As research continues to unveil their full potential, peptides are set to play a pivotal role in advancing regenerative therapies and improving patient outcomes.
- Published in Corporate News / Blog
The Future of Hair Restoration: Innovations in Regenerative Medicine
Hair restoration has come a long way, thanks to the groundbreaking advances in regenerative medicine. This field is transforming the landscape of hair restoration with cutting-edge approaches that offer promising results for those struggling with hair loss.
Stem Cell Therapy
One of the most exciting developments in hair restoration is stem cell therapy. Stem cells have the unique ability to differentiate into various cell types, including hair follicles. When introduced into the scalp, they can potentially stimulate the regeneration of hair follicles, promoting natural hair growth. This method holds great promise for those seeking a more natural and effective solution to hair loss.
Platelet-Rich Plasma (PRP)
Platelet-Rich Plasma (PRP) therapy is another innovative approach making waves in the field. PRP involves using the patient’s blood, which is enriched with growth factors. These growth factors play a crucial role in revitalizing hair follicles and improving hair growth and quality. By harnessing the body’s natural healing processes, PRP therapy offers a safe and effective way to combat hair loss.
Exosomes
Exosomes, tiny cellular vesicles, are gaining attention for their role in hair restoration. These vesicles aid in hair growth by reducing inflammation and supporting tissue regeneration. Exosomes create an optimal environment for hair follicle health, making them a valuable addition to regenerative medicine’s toolkit for hair restoration.
Why This Transformation Matters
The shift to regenerative medicine in hair restoration is significant for several reasons:
Scar Minimization
Traditional hair restoration techniques often leave visible scars. Regenerative methods, however, minimize scarring, leading to more aesthetically pleasing results. This advancement is particularly important for those concerned about the appearance of their scalp post-procedure.
Enhanced Outcomes
Patients undergoing regenerative treatments often experience more natural and robust hair growth compared to traditional methods. The integration of these advanced techniques results in fuller, healthier-looking hair, enhancing overall patient satisfaction.
Personalized Care
One of the greatest benefits of regenerative medicine is its ability to provide personalized care. Treatments can be tailored to address each patient’s specific needs and hair restoration goals. This individualized approach ensures that patients receive the most effective and appropriate treatments for their unique situations.
The Future of Hair Restoration
The future of hair restoration is bright, thanks to the integration of regenerative techniques. These methods promise more natural, minimally invasive, and personalized solutions for hair loss. As research and technology continue to advance, we can expect even more innovative and effective treatments to emerge, further revolutionizing the field of hair restoration.
In conclusion, regenerative medicine is not just transforming hair restoration—it’s offering hope and renewed confidence to those struggling with hair loss. With its potential for natural growth, minimal scarring, and personalized care, regenerative medicine is set to become the gold standard in hair restoration.
- Published in Corporate News / Blog
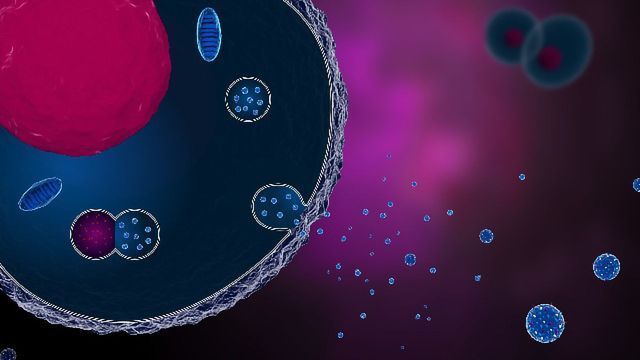
Exploring the Therapeutic Potential of Umbilical Cord Stem Cell-Derived Exosomes
In the realm of regenerative medicine, exosomes derived from umbilical cord stem cells are gaining significant attention. These nano-sized vesicles play a crucial role in cell-to-cell communication and have shown immense therapeutic potential. This article delves into the origins, functions, and promising applications of umbilical cord stem cell-derived exosomes.
What Are Exosomes?
Exosomes are small extracellular vesicles, typically 30-150 nm in diameter, secreted by various cell types. They are involved in intercellular communication, transferring proteins, lipids, and nucleic acids between cells. Exosomes are known to influence numerous physiological processes, including immune responses, inflammation, and tissue repair.
Umbilical Cord Stem Cells: A Rich Source
Umbilical cord stem cells, particularly mesenchymal stem cells (MSCs), are a rich source of exosomes. These stem cells are easily accessible, and have a high proliferative capacity. The exosomes derived from umbilical cord MSCs are packed with bioactive molecules that exhibit potent regenerative properties.
Mechanism of Action
Exosomes exert their therapeutic effects through several mechanisms:
- Cellular Communication: Exosomes facilitate communication between cells by transferring bioactive molecules, which can modulate the behavior of recipient cells.
- Anti-inflammatory Effects: They help reduce inflammation by modulating the immune response.
- Tissue Repair and Regeneration: Exosomes promote tissue repair by enhancing cell proliferation, migration, and differentiation.
Therapeutic Applications
1. Wound Healing
Exosomes from umbilical cord stem cells have shown to accelerate wound healing by promoting angiogenesis (formation of new blood vessels), collagen synthesis, and reducing scar formation.
2. Cardiovascular Diseases
Studies have demonstrated that exosomes can improve cardiac function following myocardial infarction by enhancing cardiac cell survival, reducing fibrosis, and promoting angiogenesis.
3. Neurological Disorders
Exosomes have the potential to treat neurodegenerative diseases such as Alzheimer’s and Parkinson’s by delivering neuroprotective agents, reducing neuroinflammation, and promoting neuronal survival.
4. Liver Diseases
Exosome therapy is emerging as a promising treatment for liver diseases. They can help in the regeneration of liver tissue, reduce fibrosis, and improve overall liver function.
5. Orthopedic Applications
In orthopedic medicine, exosomes can aid in the healing of bone fractures, cartilage damage, and osteoarthritis by promoting the differentiation of stem cells into bone and cartilage cells.
6. Aesthetic Uses
Exosomes derived from umbilical cord stem cells are making waves in the field of aesthetics for their skin rejuvenation capabilities. They can:
- Promote Collagen Production: Leading to firmer, more youthful-looking skin.
- Enhance Skin Elasticity: Improving skin texture and reducing fine lines and wrinkles.
- Accelerate Skin Repair: Aiding in the healing of acne scars and other skin blemishes.
- Reduce Inflammation: Helping to calm irritated skin and reduce redness.
Clinical Trials and Research
Numerous clinical trials are underway to evaluate the safety and efficacy of exosome-based therapies. These studies are exploring a wide range of applications, from treating chronic wounds to regenerative treatments for heart disease and aesthetic improvements.
Future Perspectives
The field of exosome research is rapidly evolving. Advances in isolation techniques, molecular profiling, and delivery systems are expected to enhance the therapeutic potential of exosomes. Personalized medicine, where exosomes are tailored to the needs of individual patients, is a promising future direction.
Challenges and Considerations
While the potential of exosome therapy is immense, several challenges need to be addressed:
- Standardization: Developing standardized protocols for exosome isolation, characterization, and storage.
- Safety: Ensuring the safety and minimizing the risk of adverse effects.
- Scalability: Producing exosomes on a large scale for clinical use.
Conclusion
Exosomes derived from umbilical cord stem cells hold immense promise in regenerative medicine, aesthetic treatments, and disease management. Their ability to modulate cellular communication and promote tissue repair makes them a powerful tool for various therapeutic applications. As research progresses, the translation of exosome therapy from bench to bedside is becoming increasingly feasible, heralding a new era in medical treatment.
- Published in Corporate News / Blog
New advances in osteoarthritis therapy with stem cells
Osteoarthritis is a rheumatic pathology that damages the articular cartilage. By joining two bones through the joint capsule, the joints are able to move, providing us with functional autonomy. An inner fluid called synovial fluid is usually found within joints, which is produced by the synovial membrane. Articular cartilage covers the ends of the bones that form the joint. As a result of damage to this articular cartilage, pain, stiffness, and functional impairment occur. Osteoarthritis is the most common joint disorder, usually beginning between the ages of 40 and 50, affecting to some degree almost everyone over the age of 80. Typically, osteoarthritis affects the spine, shoulders, fingers, hips, knees, and toe joints.
Stem cell therapies have the potential to treat a broad spectrum of diseases. Whether it’s rhizarthrosis, diabetes, neurodegenerative diseases, spinal cord injuries, or heart disease. By utilizing stem cells, regenerative medicine is capable of repairing tissues in affected areas. The main difference between lipo gem therapy and other treatments for osteoarthritis is that lipogem therapy regenerates cartilage, avoids surgery and its sequelae, and improves the quality of life for patients.
The potential for medical treatments with stem cells and their by-products is currently very high. In the field of sports medicine and traumatology, one of the most outstanding advances has been made for the first time in decades recently: Spanish scientists have achieved a degree of tendon regeneration in 100% of injured patients, resulting in a decrease in pain and a return to sport within two months, and just six months after the trial was completed.
A research performed by the Institute of Regenerative Tissue Therapy (ITRT), published by the prestigious American Journal of Sports Medicine. Demonstrates how this therapy regenerates chronic lesions in the patellar tendon and opens up a new therapeutic option for this tissue, which was considered impossible to regenerate.
In most patients, fat tissue can be harvested minimally invasively (under local or general anesthesia), providing a highly viable MSC population regardless of donor age. Similar to MSCs derived from other tissues, adipose tissue-derived MSCs have regenerative potential. As osteoarthritis is a very common joint disease, and knee osteoarthritis is the most common form, it is necessary to review scientific literature on osteoarthritis treatments with stem cells, like lipogems.
Lipogems Therapy
Lipogems therapy is a novel procedure that enhances the body’s natural ability to heal itself through the innovative power of science and biotechnology. The Lipogems method involves injecting mesenchymal stem cells into the joints. Adipose-derived mesenchymal stem cells have enormous regenerative potential. They also have a regenerative capacity independent of their age. Even older individuals can benefit from this procedure.
Injection of mesenchymal stem cells into the knee, particularly in the early stages of osteoarthritis, can stop the process of inflammation and degeneration, especially in the less advanced stages of the disease. In addition to preventing progressive physical deterioration of the articular cartilage, this treatment contributes significantly to a patient’s well-being and prevents the installation of knee prostheses.
Patellar tendinopathy, physiotherapeutic treatment and stem cell therapy
Injuries to the patellar tendon that connects the kneecap to the tibia are known as patellar tendinopathy or patellar tendinitis. The patellar tendon works with the muscles in the front of the thigh to extend the knee so you can kick, run and jump. Athletes who perform frequent jumping in their sports, such as basketball and volleyball, are most likely to suffer from patellar tendonitis. However, people who don’t engage in jumping sports may develop patellar tendonitis. Patients with patellar tendinitis usually begin treatment with physical therapy to stretch and strengthen their knee muscles.
Strength training with eccentric resistance is one of the most common treatments for tendinopathies. Alternatively, it has been demonstrated that bone marrow-derived mesenchymal stem cells (MSCs) can regenerate injured patellar tendons. Within six months of treatment, it has been observed that the structure of this tissue – which is always difficult to treat – is restored, reaching a regeneration of 40% in all injured persons, with a gradual improvement that eventually becomes complete.
It has been found that traditional management methods, including isometric or eccentric exercises, shock wave therapy, and even surgery, are not effective. As part of a rehabilitation program in chronic patellar tendinopathy, autologous expanded bone marrow mesenchymal stem cells (BM-MSC) or leukocyte-poor platelet-rich plasma (Lp-PRP) may be effective in reducing pain and improving activity levels. Traditional management, which includes isometric or eccentric exercises, shock wave therapy, and even surgery, has limited success. A combination of autologous expanded bone marrow mesenchymal stem cells (BM-MSCs) and leukocyte-poor platelet-rich plasma (Lp-PRP) and rehabilitation may reduce pain and improve activity levels in active participants with chronic patellar tendinopathy.
To learn more about stem cells, cellular therapies and keep up to date with all the information about regenerative medicine and its advances, sign up for our international certification in regenerative medicine at www.issca.us
- Published in Corporate News / Blog
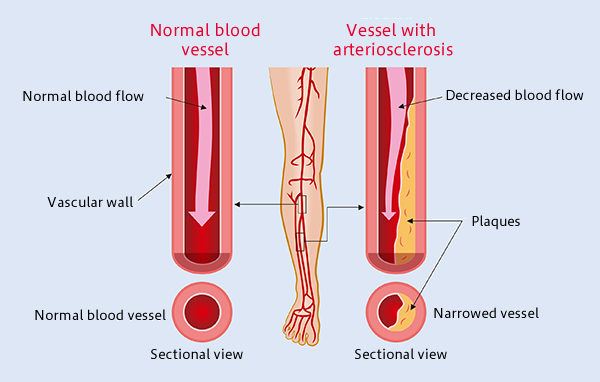
Atherosclerosis: The Most Common Form of Arterial Occlusive Disease in Adults
Introduction to Atherosclerosis
Atherosclerosis is the most common form of arterial occlusive disease in adults. About 15 percent of adults over 55 years of age suffer from critical ischemia, the most severe form of this disease.
Due to the gradual aging of the population and the growing number of people in their third age group, a number of studies have been conducted in order to improve the prognosis of atherosclerosis obliterans and to find alternatives to the mutilation of the extremities. As a general rule, chronic ischemia of the lower limbs should be treated to alleviate symptoms, particularly pain, prevent disease progression, and reduce the rate of amputations. In most patients with critical ischemia, the main goal is to preserve the affected limb.
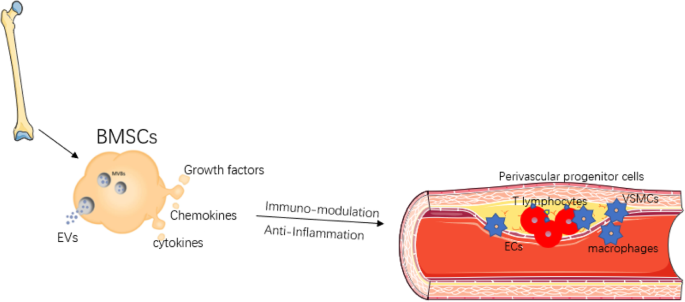
Atherosclerosis Obliterans Grade IV
The development of regenerative medicine is closely linked to the development of new knowledge about embryonic and adult stem cells, as well as the regenerative and therapeutic potential of stem cell therapy. The use of adult stem cells in the treatment of peripheral artery diseases has been demonstrated as a therapeutic agent for inducing angiogenesis. Recent preclinical studies, as well as pioneering clinical studies, indicate that bone marrow-derived mononuclear cells (MBMCs) can enhance tissue vascularization in ischemic limbs, with results similar to those obtained with peripheral blood stem cells supply.
Case Studies and Research
Cuba presented the first studies carried out in 2004 at the Institute of Hematology of the “Enrique Cabrera” hospital in Havana City, which achieved encouraging clinical results and had very few adverse effects in recent years.
A progressive rise in the accumulated experience with stem cells was also observed in Pinar del Rio in 2005, as the first 10 cases were carried out. The rising ease of obtaining this type of cell has made research and applications with these cells advance rapidly with great expectations in terms of clinical application.
Research Findings on Atherosclerosis Obliterans Grade IV
A study published by Dia-Diaz, et al. in the Journal of Medical Sciences of Pinar del Rio examined 296 patients with grade IV atherosclerosis obliterans between 2009 and 2019. During the study, autologous stem cells were injected intramuscularly from peripheral blood. Within four weeks, pain relief was observed, as well as an increase in the pain-free claudication distance. Angiography after treatment revealed collateral vessel formation. The limb was saved in 201 patients (68%), while 95 cases (32%) presented amputation criteria. Complications were not reported following the procedure.
The study demonstrated the effectiveness of the implantation of autologous stem cells obtained from peripheral blood, as well as the favorable evolution of patients, clinical improvement of rest pain, walking distance without claudication, and ankle-brachial pressure index.
We still need to explore a lot of ground in terms of these and other conditions. You can learn more about regenerative medicine and stem cells by enrolling in our international certification program at www.issca.us.
- Published in Corporate News / Blog
How Exosome Therapy Differ from Stem Cell Therapy
Exosomes are potent microvesicles released by adult mesenchymal stem cells. They have the ability to help restore cells in the body by improving cell to cell communication.
Exosomes are not cells, and they are smaller than cells. When compared to adult stem cells, exosomes have much more growth factors which give them a better clinical and aesthetic potential than stem cells.
It’s a cell-free cell therapy, this makes it safer compared to other cellular therapy, because there’s no risk of rejection in graft Vs host.
Unlike some other cellular therapies, exosomes do not produce host graft reactions, because they do not carry HLA genetic information and are not cells but extracts of the cells (released by cells).
Exosomes have a superior regenerative capacity, because they are obtained from newborn umbilical cord tissue mesenchymal cells, which means they have not been exposed to any contaminating or toxic agent because our cells are as healthy as our body.
Exosomes improve the signaling between cells, thereby making them useful to revitalize, rejuvenate, restore, and cause anti-inflammatory effects in the body.
When compared to autologous adult stem cells, exosomes have much more healthy growth factors which gives them a better clinical and aesthetic potential than stem cells.
Exosomes are less complicated products to transport because the cells used in cellular therapy must be applied to the patient very quickly because they are live cells. In the laboratory, once they are thawed the doctors have limited time to apply them. However, with exosomes, they last longer, because as they are proteins they do not denature and can last for longer periods.
Exosomes is a superior product to autologous treatments because they do not require a surgical procedure, they come in a vial that can be injected directly, significantly reducing the risk and complications of a surgical procedure.
It is a superior product to autologous stem cell therapy because the patient’s cells have the same age and the same quality. For example, if a patient is a smoker and intoxicated, obviously the health of his cells is not the best. That is why the most indicated product is a donor product that is pure and free of toxins.
Mesenchymal cell-derived exosomes are preferably used in regenerative medicine. These cells are excellent regenerative cells due to their multipotent nature, therefore MSCs derived exosomes are superior to other exosomes products.
The Cellgenic lyophilized exosomes are derived from mesenchymal cells, which makes it superior to other exosome products, because mesenchymal cells have superior and excellent regenerative capacity.
This is why exosome therapy, especially Cellgenic lyophilized exosomes should be a doctor’s first choice.
- Published in Corporate News / Blog
How much does exosome therapy cost?
Exosome therapy is the new buzz in the regenerative medicine industry because of how it can repair and regenerate your cells and tissues.
Exosome therapy is safer compared to other cellular therapy because it’s a cell-free therapy with no risk of rejection.
Exosome therapy will be beneficial to you if you’re dealing with conditions such as sports injuries, tissue regeneration, hair loss, erectile dysfunction, chronic pain, and many other applications.
In this article, you’ll learn about the cost of exosome therapy and how you can benefit from it.
How the Cost of Exosome Therapy is Determined
All cells produce exosomes, which are microvesicles that contain biochemical and genetic information.
The cost of an exosome product (used in exosome therapy) will depend on the type of cell line (raw tissue source) used to extract the exosomes.
The first factor to determine the cost of an exosome product is the quality of the tissue source.
The most commonly used tissue types are cord blood, amniotic fluid, and mesenchymal cell cultures.
Exosomes derived from mesenchymal cell cultures are the most difficult to obtain but offer the greatest therapeutic potential.
How Much Does Exosome Therapy Cost?
The average cost of exosome therapy is $4,900, but the price can range from $3,500 to $6,500.
It’s also important to note that the price depends on your specific needs and your treatment plan, as decided by the doctor.
The doctor will schedule a consultation with you to determine your personalized treatment plan.
The exosome therapy can either be given as an IV infusion or as localized injections, depending on the purpose of the therapy.
Exosomes are very useful to revitalize, rejuvenate, restore, and reduce inflammations in the body.
Benefits of Exosome Therapy
Hair Loss Therapy
If you’re in the early stages of hair loss, exosome therapy can help regenerate your hair whether you’re a man or woman. After exosome therapy, you’ll start seeing new hair growth in as little as two to three months, with significant results showing six months to one year later.
Chronic Pain
If you’re experiencing chronic pain due to degenerative conditions such as arthritis, exosomes can help subdue the pain by regenerating the cells and helping the body work better.
Degenerative Conditions
For degenerative medical conditions such as osteoarthritis and musculoskeletal injuries, exosome therapy can help your body repair the damage done to your cells, prevent further deterioration, and help you feel better.
Skin Therapy
Exosome therapy can reduce inflammation in the skin by improving its strength and elasticity.
Anti-Aging
If you would like to retain your youthful glow, exosome therapy can make you feel young again by rejuvenating your skin and reversing the aging process in your cells.
Where Can You Get Exosome Therapy?
Cellular Hope Institutes provide exosome therapy for patients looking for better outcomes for various conditions.
The exosomes used at Cellular Hope Institute are obtained from umbilical cord tissue discarded after birth, which means these exosomes have not been exposed to any contaminants or toxic agents, ensuring a higher capacity to regenerate your cells and tissues.
- Published in Corporate News / Blog
Culture Expanded MSCs
Mesenchymal Stem Cells (MSCs) are the most commonly used cells in stem cell therapy and regenerative medicine due to their high multi-potency. MSCs can be isolated from different tissues in the body.
In this article, you’ll learn about culture-expanded MSCs, how MSCs can be expanded, the potency of MSCs, and the types of cells they can differentiate into.
What Are Culture Expanded Mesenchymal Stem Cells?
Mesenchymal stem cells are highly potent cells used for cellular therapy and are isolated from different parts of the body. MSCs can be used to improve patient outcomes in diseases and conditions such as autoimmune diseases, degenerative diseases, nerve damage, diabetes mellitus, bone problems, etc.
For every patient, millions of MSCs are needed, and the exact amount varies according to disease, route of administration, administration frequency, weight, and age of the patient.
MSCs are expanded in a culture medium on a large scale to obtain the required quantity of cells needed for cellular therapy.
Culture Expanded MSCs: How Does It Work?
Expanding MSCs in a medium involves a step-by-step process of isolation and expansion.
Mesenchymal Stem Cells Isolation
MSCs can be isolated from different tissues in the human body such as adipose tissues, dental pulp, human bone marrow, umbilical cord tissue, umbilical cord blood, peripheral blood, and synovium.
MSCs are expanded in culture to increase their yield and amplify their desired functions and potency.
Although the population of MSCs obtained will vary from donor to donor, here are some steps to follow:
- Acquire fresh tissue extracts in strictly aseptic conditions to maintain purity.
- To remove any cell clusters, filter the cell suspension with a 70-mm filter mesh.
- Use a centrifuge to roll the cells for about 5 minutes at 500g.
- Suspend the cells again to measure the cell viability and yield using Trypan blue exclusion.
- Use T75 culture dishes to culture the cells in 10 mL of complete MSC medium at a density of 25 × 10^6 cells/mL. Incubate the plates at 37°C with 5% CO2 in a humidified chamber without any interruption.
- After 3 hours, remove the non-adherent cells by changing the medium and replacing it with 10 mL of fresh complete medium.
- After an additional 8 hours of culture, add 10 mL of fresh complete medium as a replacement for the existing medium. Repeat this step every 8 hours for up to 72 hours of initial culture.
- Cells can be frozen in MSC growth media plus 10% DMSO (D2650) at a density of 2X10^6 cells/vial.
Expansion of Mesenchymal Stem Cells in a Culture Medium
Culture-expanded MSCs undergo various stages from the preparation of the culture plate, thawing of MSCs, and the actual expansion of MSCs.
The reason behind the cultural expansion of MSCs is to get them to differentiate into other cell types such as osteoblasts, adipocytes, and mesenchymal stromal cells.
Preparation
To expand MSCs in a culture medium, you need culture ware. You can get one plastic or glassware plate and coat it with a sufficient amount of 0.1% gelatin. Don’t forget to aspirate the gelatin solution from the coated plate or flask before you use it.
Thawing of Mesenchymal Stem Cells
- After the recommended culture medium and coated culture ware is ready and on standby, remove the vial of MSCs from liquid nitrogen and incubate in a 37°C water bath until all the cells are completely thawed. The extent of completely thawed frozen cells and how fast they thaw determines cell viability.
- Once the cells have thawed completely, disinfect the walls with 70% ethanol before proceeding to the next step.
- Place the cells in a hood, and carefully transfer the cells to a sterile tube with a pipette (1 or 2 mL pipette), doing this to prevent bubbles.
- Add drops of MSC expansion medium that have been pre-warmed to 37°C to the tube containing the MSCs.
- Mix the suspension slowly by pipetting up and down two times while avoiding any bubbles.
- Place the tube in a centrifuge and centrifuge the tube at 300 x g for 2-3 minutes to roll the cells, avoiding vortexing the cells.
- Decant as much of the supernatant as possible to remove residual cryopreservative (DMSO).
- Suspend the cells in a total volume of 10 mL of MSC Expansion Medium again or any alternative of choice, pre-warmed to 37°C, containing freshly added 8 ng/mL FGF-2 (F0291).
- Place the cell suspension onto a 10-cm tissue culture plate or a T75 tissue culture flask.
- Maintain the cells in a humidified incubator at 37°C with 5% CO2.
- The next day, exchange the medium with fresh MSC Expansion Medium (pre-warmed to 37°C) containing 8 ng/mL FGF-2. Replace with fresh medium containing FGF-2 every two to three days thereafter.
- Isolate the cells when they are approximately 80% confluent, using Trypsin-EDTA, and passaged further or frozen for later use.
Functions of Culture Expanded MSCs
MSCs are required to be expanded in order for them to be used clinically for therapeutic purposes.
Culture-expanded MSCs can be induced to differentiate into adipocytes, osteocytes, hepatocytes, chondrocytes, tenocytes, and cardiomyocytes.
Due to their potential to differentiate into different kinds of cells in the body, MSCs can be used to manage liver problems, heart problems, joint and bone problems, etc.
MSCs are also used in tissue regeneration and modulation of the immune system. They possess anti-apoptotic, angiogenic, anti-fibrotic, and anti-oxidative properties.
However, the quantity of MSCs isolated from body tissues is not enough for clinical and therapeutic applications.
This is why MSCs are expanded in culture to increase their yield for desired therapeutic effect.

- Published in Corporate News / Blog
Why cellular therapies have become a standard in clinics that are betting on biological medicine
Cellular therapy is fast becoming a standard therapy in many regenerative clinics today. Many doctors are no longer questioning the safety and effectiveness of stem cell therapy. This is because various stem cell studies are already describing the benefits of stem cells for patients who are living with chronic and autoimmune health conditions.
This article will discuss why stem cell therapy has become a standard therapy in clinics, the paracrine effect of stem cells, and other reasons why doctors are adopting stem cells in their clinics.
Benefits of Stem Cell Therapy
Stem cell therapy is an important innovation in medicine because of its regenerative power in the human body. Most disease states are characterized by damaged cells, tissues, and organs, which is where stem cell therapy comes in. In stem cell therapy, stem cells are administered into the human body and replace the cells damaged by disease or health disorders.
Stem cell research has revealed two major ways of using stem cells to rebuild defective and damaged cells. One of these ways can be seen in procedures like bone marrow transplant, where stem cells are used to replace the damaged cells by engrafting, and they then differentiate into the proper cell type. Another mechanism relies on the paracrine effect of stem cells. This procedure of stem cell therapy involves using stem cells isolated from a donor to stimulate the patient’s cells to repair damaged tissues.
Additionally, unlike traditional therapy, stem cells have a wide application. Stem cell therapy is used to manage various degenerative diseases, autoimmune disorders, birth defects, and the research is still ongoing for so many other health conditions where stem cells have shown potential.
Also, there is currently a high demand for aesthetic medicine. Stem cell therapy is a proven alternative to other forms of cosmetology such as plastic surgery. Hence, dermatologists are turning to stem cell therapy to administer anti-aging procedures, skin rejuvenation, hair therapy, micro-needling, etc.
Why Cellular Therapies Have Become a Standard
The paracrine effect of stem cells is one of the most outstanding effects of stem cells. It involves using donor cells to stimulate endogenous repair by harnessing the regenerative power of the human body. It is a mechanism of tissue regeneration that has created new possibilities for managing various conditions using stem cell therapy.
The cells that trigger a paracrine response are mesenchymal cells, umbilical cord blood, umbilical cord tissue, adipose (fat) tissue, and blood cells from a donor’s bone marrow.
The Paracrine Effect of Stem Cells
The paracrine effect occurs when the donor’s cells send the damaged or defective cells signals to induce self-regeneration and repair by secreting some factors and proteins. One of the mechanisms by which this paracrine effect is initiated involves the secretion of cytokines and regulatory proteins by the damaged patient’s cells. These cytokines and proteins act as mediators to stimulate an immune response that attracts the donor cells, causing the donor cells to release proteins and factors that stimulate the patient’s cells to promote cell proliferation, increase vascularization, and blood flow to the areas that need to heal, while reducing inflammation.
Moreover, research has shown that the paracrine effect of stem cells prevents damaged and diseased cells from dying. They are also therapeutically useful in autoimmune diseases and preventing transplant rejection due to the immune suppression effect they have.
Is Stem Cell Therapy Effective?
Doctors are always looking for ways to provide the best possible treatment to their patients, and that is why many clinics are embracing stem cell therapy as a standard, due to its many advantages.
Stem cell therapy is one of the most effective and safest therapies patients can receive compared to other existing treatment options. Stem cell therapy is used in promoting patient outcomes in a lot of disease conditions that were previously poorly treated by other alternatives.
As new potentials and ways of applying stem cells are being discovered, doctors are beginning to maximize these benefits in their clinics. Some conditions that are currently treated by stem cells include autoimmune conditions, immunotherapy CAR-T cells, chronic obstructive pulmonary disease, neurodegenerative conditions, osteoarthritis, spinal cord injury, aesthetics/anti-aging, sports medicine, autism, and multiple sclerosis.
Therapeutic Uses of Stem Cells vs Traditional Medicine
Existing stem cell research has shown how the regenerative effect of stem cells is defining the future of medicine. The major advantage of stem cell therapy over conventional medication-based therapy is its safety. Stem cell therapy is aimed at treating the cause of the disease while traditional medicine targets the symptoms.
Another problem with traditional medical therapy is that it introduces another problem while trying to solve the existing one. As a doctor, you always run the risk of causing harm with each prescription because of various adverse effects that could lead to major organ damage of the kidney, liver, etc. On the other hand, patients already know this and they are actively seeking better alternatives, which is why stem cell therapy is fast becoming a standard therapy in clinics.
Moreover, doctors will always be concerned about whether their patients are taking their medications or not. The burden of drug compliance and adherence associated with traditional medical therapy is not always easy to navigate. This is why effective treatment options like stem cell therapy have become a standard therapy in clinics. It only requires the patient having a procedure that repairs and restores damaged cells and tissues in the most natural way.
If you would like to become certified in regenerative medicine using stem cells and other cellular therapy, contact us.
- Published in Corporate News / Blog